Other Rare ILDs
ILDs which don’t fit into the other categories are listed on this page.
EOSINOPHILIC PNEUMONIA
DISEASE DEFINITION
Characterized by presence of eosinophils in alveolar spaces, BAL fluid, and/or the interstitium.1
Acute:1,2
- Unknown etiology characterized by rapid eosinophilic infiltration of the lung interstitium
- Can be caused by tobacco exposure, medications, fungal/parasitic infection
Chronic:3
- Acute or subacute illness that recurs
- May be allergy related
EPIDEMIOLOGY AND RISK FACTORS
Prevalence and incidence of eosinophilic pneumonia is unknown:
Acute:1,2
- Often affects otherwise healthy male patients, usually smokers, 20 to 40 years of age
Chronic:3
- Most patients are nonsmokers
- Patients may have allergy or asthma history3
DIAGNOSIS
SYMPTOMS
Acute:1,2
Patient presents with an acute febrile illness (duration <7 days) and acute respiratory failure requiring mechanical ventilation:
- Nonproductive cough
- Dyspnea
- Malaise
- Myalgias
- Night sweats
- Pleuritic chest pain
- Tachypnea
- Fever (>38.5°C)
- Bibasilar inspiratory crackles
- Rhonchi on forced exhalation
Chronic:3,4
Patient presents with sudden and severe illness characteristic of community-acquired pneumonia:
- Cough
- Fever
- Progressive dyspnea
- Wheezing
- Night sweats
- Weight loss if symptoms are recurrent
DIAGNOSTIC TESTS
| Acute:1,2 | |||||||||
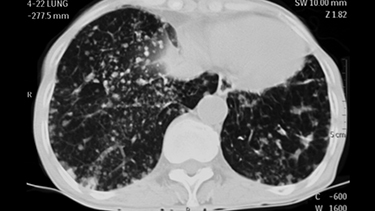
| Imaging — CXR and HRCT |
|
||||||||
| CBC |
|
||||||||
| Pleural fluid analysis |
|
||||||||
| PFTs |
|
||||||||
| Bronchoscopy/BAL/biopsy |
|
||||||||
| Chronic:3,4 | |||||||||
| CXR |
|
||||||||
| CBC, ESR, iron studies |
|
||||||||
| BAL |
|
||||||||
DIAGNOSIS OF ACUTE EOSINOPHILIC PNEUMONIA1
- Acute respiratory illness (duration <1 month)
- Pulmonary infiltrates on imaging
- Pulmonary eosinophilia (>25% eosinophils in BAL fluid) or eosinophilic pneumonia on lung biopsy
- Absence of other specific pulmonary eosinophilic diseases
DIAGNOSIS OF CEP4
- Respiratory symptoms (duration >2 weeks)
- Alveolar and/or blood eosinophilia
- Peripheral pulmonary infiltrates on imaging
- Exclusion of any known causes
MANAGEMENT1,2,3,4
Acute:1,2
- Systemic corticosteroids; if applicable, remove identified trigger or exposure
- Prognosis is usually good
- Patients commonly respond to corticosteroids with full recovery
- Resolution of symptoms within 24-48 h, radiographic abnormalities within 30 d
Chronic:3,4
- Systemic corticosteroids
- Maintenance therapy: inhaled corticosteroids, oral corticosteroids, or both
- Failure to respond (within 48 h) to steroids suggests another diagnosis
- Resolution of symptoms and radiographic abnormalities in 14-30 d
NEUROFIBROMATOSIS
DISEASE DEFINITION
- 3 major forms: type 1 (NF1), type 2 (NF2), schwannomatosis5,6
- NF1 (von Recklinghausen disease) is the most common type and also exhibits thoracic manifestations7
EPIDEMIOLOGY
- NF1 is an autosomal dominant genetic disorder with an incidence of approximately 1 in 2600 to 3000 individuals5,8
- Approximately 5% of NF1 patients develop mediastinal tumors7
- A total of 64 cases of NF-associated diffuse lung disease have been identified9
DIAGNOSIS OF NF18
- Presence of ≥6 café au lait macules, >5 mm in diameter pre-puberty or ≥1.5 mm post-puberty
- Skin-fold freckling
- ≥2 neurofibromas or 1 plexiform neurofibroma
- ≥2 iris hamartomas (Lisch nodules)
- Optic glioma
- Skeletal dysplasia
- Affected first-degree relative
SYMPTOMS OF NEUROFIBROMATOSIS WITH DIFFUSE LUNG DISEASE (NF-DLD)9
Dyspnea in 80% of patients
Cough in 32% of patients
Chest pain in 5% of patients
11% of patients are asymptomatic
THORACIC MANIFESTATIONS10
- Neurofibroma: well-circumscribed round or elliptic masses in the paravertebral regions or along the nerves’ courses
- May erode, invade, or destroy adjacent bone; may calcify
- Focal thoracic scoliosis
- Posterior vertebral scalloping
- Enlarged neural foramina
- Characteristic rib abnormalities — due to bone dysplasia or erosion from adjacent neurofibromas
- Lung Parenchymal Disease11
- Cysts and bullae formation: upper lobe
- Diffuse interstitial fibrosis: lower lobe
- Ground-glass opacification
- Basilar reticular abnormalities
- Secondary Pulmonary Arterial Hypertension12
MANAGEMENT8
- Aims at early detection and symptomatic treatment of complications as they occur
- The decision to obtain testing such as imaging studies depends on the history and physical findings
- There is no overall treatment for NF1 or any therapeutic agents specifically approved for patients with NF1